Brain-Computer Interfaces and Neurorestoration
- Mijail Serruya
- Sep 27, 2025
- 4 min read
PART 1: OVERVIEW
Pioneering Brain-Computer Interfaces and Neurorestoration
I lead the Raphael Center for Neurorestoration at Thomas Jefferson University, where we're advancing from proof-of-concept to clinical deployment of technologies that restore function after neurological injury.
Background: My work in brain-computer interfaces began in 1998 in John Donoghue's lab at Brown, where we published the first demonstration of instant neural cursor control in Nature. I helped co-found Cyberkinetics, helped design the BrainGate trial with Matt Nagle—the first person with a chronic multi-electrode implant—and contributed to foundational work showing neural control of prosthetics, published in Nature in 2006.
Current Impact: Since joining Jefferson in 2011, I've built a multidisciplinary team conducting FDA-regulated first-in-human trials:
Cortimo trial (2018-2022): First brain-computer interface for stroke rehabilitation, linking motor cortex signals to powered orthosis ($500K seed funding from Jefferson leadership)
NuroSleeve: User-centered 3D-printed assistive system now in daily home use by participants
RISES: $4M Reynolds Foundation-funded open-source closed-loop stimulation platform for spinal cord injury

Team Capabilities: Seven-person core team (engineering, software, electrophysiology, machine learning, patient navigation) plus expanding network. We've built FDA V&V workflows, maintain active partnerships with Precision Neuroscience and MicroTransponder, and generate ~$500K/year in philanthropic and corporate support.
Innovation Pipeline: Moving three tracks in parallel: (1) near-term: commercializing NuroSleeve with entrepreneur-in-residence; (2) mid-term: iBCI-ready platforms compatible with any FDA-approved implant; (3) long-term: "virtual white matter" connecting multiple neural tissue specimens, creating biological computing substrates and potentially enabling peritoneal "neo-brains" to augment injured cerebral tissue.
Vision: We're building an ecosystem spanning immediate assistive devices through living neural interfaces—combining synthetic and biological components to literally reconstruct the injured brain and restore independence.
PART 2: DETAILED NARRATIVE
From Undergraduate Research to iBCI Pioneer
My path began at Brown University (1992-2005) studying thalamocortical physiology with Barry Connors as an undergraduate, followed by Fulbright work on electrophysiology in Jerusalem. During MD/PhD training, I joined John Donoghue's lab—meeting future leaders like Nicho Hatsopoulos (University of Chicago), Liam Paninski (Columbia), and Mikhail Shapiro (Caltech). My doctoral work demonstrated instant neural control of cursor movements purely from thought, published in Nature 2002.
This led to co-founding Cyberkinetics with Nandini Murthy, where we raised $5M (including $1M angel investment from Oxford Bioscience) and designed the landmark BrainGate trial. Working with Matt Nagle, a tetraplegic volunteer whose altruism we honor, we published the first demonstration of chronic multi-electrode array control of prosthetics (Nature 2006). I led experiments showing neural control of TV channels, drawing, prosthetic hands, and robotic arms, with software by Dan Morris (now at Microsoft).
After neurology residency at Penn (with intracranial EEG work revealing memory signatures published in Cerebral Cortex), I joined Jefferson in 2011, building the first cognitive neurology clinic, then concussion care and integrative brain health programs.
Cortimo & NuroSleeve
In 2018, Robert Rosenwasser (neurosurgery chair and endovascular pioneer) provided $500K seed funding for our first trial: implanting an intracortical BCI in cortex overlying chronic basal ganglia stroke, linking outputs to a wearable powered orthosis. Volunteer Aaron Ulland revealed unprecedented neural signatures in stroke-affected cortex, published in Communications Medicine 2022 and analyzed in Frontiers in Human Neuroscience 2025.
Aaron's feedback that the orthosis was uncomfortable and limited led us to industrial designer Mikael Avery. Together with occupational therapy experts and scientists MJ Mulcahey and Namrata Grampurohit, we developed NuroSleeve through an iterative clinical trial where each participant benefited from prior lessons. Participants returned for final designs now in daily home use (published Journal of NeuroEngineering and Rehabilitation 2023, Archives of Rehabilitation Research and Clinical Translation 2023). IP filed, and we have partnered with a superb entrepreneur-in-residence, Matt Adams.
Expanding the Platform
Through Dr. Alex Vaccaro's introduction, we won $4M from Reynolds Foundation for RISES—an open-source closed-loop spinal cord stimulation platform. Our work revealed critical insights about electrode spatial location (Bioengineering 2025). This established our FDA-ready device design workflow.

We've explicitly designed FREEDOM platform as "iBCI-ready"—compatible with any FDA-approved implant to control NuroSleeve, RISES, home robotics, and adaptive positioning (wheelchair seat, medical bed, drinking straw, etc). Partnership with Precision Neuroscience enables analysis of rich cortical surface datasets from surgical participants.
Beyond Traditional BCIs: Living Interfaces
While advancing conventional devices, we're pioneering biological substrates:
Virtual White Matter (Journal of Neural Engineering 2025): Connects multiple neural tissue specimens across space via software, enabling complex circuit assemblies with robustness. Proof-of-concept demonstrates real-time linking of human in vivo intracranial activity to in vitro tissue.

Biological Computing Applications:
Mapping optimal electrical stimulation patterns to determine how neural tissue exhibits "adaptive response functions"
Virtual embodiment of tissue specimens in robotic environments
Potential FDA application: autologous "living neural twins" for de-risking clinical trials
Ultimate goal: connecting in vivo brain to unlimited external neural tissue via virtual white matter

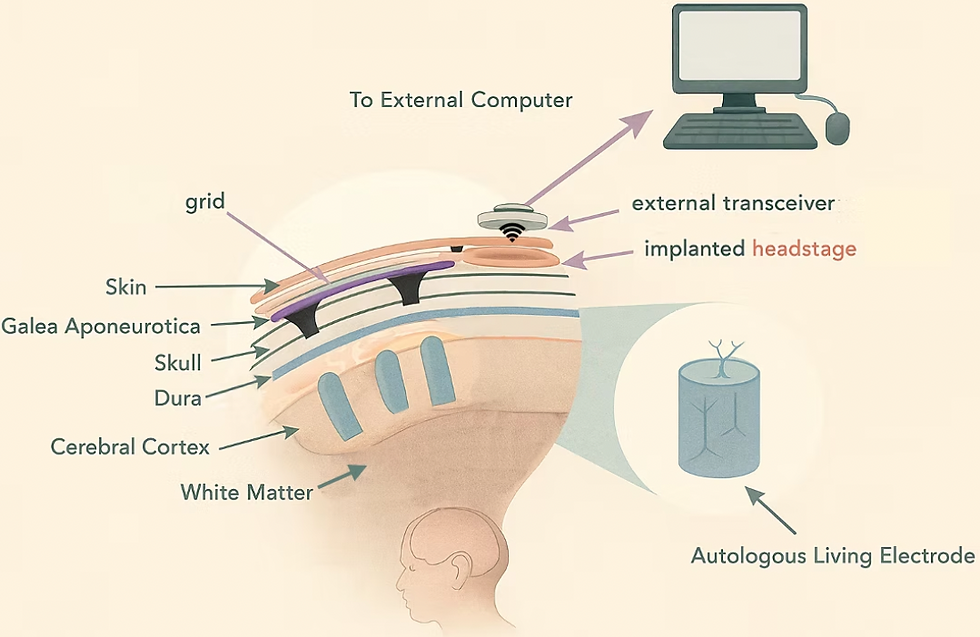
Living Medical Devices: Drawing on Kacy Cullen's "living electrodes" (Penn), Todd Kuiken's targeted muscle reinnervation, and Paul Cederna/Cindy Chestek's regenerative peripheral nerve interfaces, we envision:
Living electrodes topped with living amplifiers (myocytes or engineered electrocytes)
Temporal integrators shifting gamma frequencies down through skull's low-pass filter
Living antennae and multiplexers sampling wide brain volumes
"Neo-spinal-cord" conduits: axonal bundles connecting cortical implants directly to distal spinal cord or muscles
Peritoneal "neo-brains": vascularized assembloids in abdomen connected via biological conduits, providing more volume and better heat dissipation than skull

Clinical Translation Philosophy: "Find Them and Guide Them"
Experience with Cortimo revealed discontinuity in chronic stroke care. While acute intervention is optimized, patients go home to fragmented follow-up. Our AI pipelines process unstructured EHR text to identify treatment candidates, while software tools help patient navigators work efficiently in cybersecure environments.
Team Expertise:
Alessandro Napoli, PhD (Director of Engineering): Multi-talented engineering, team management, financial oversight
Phyo Thuta Aung (software lead): Multiprocessing, systems integration
James Lim (neurophysiologist): Neural signal analysis, in vitro electrophysiology and tissue culture
Michael Trakhtorchuk (PT/engineering): Exercise physiology, device fabrication and testing, 3D design and printing
Nabila Shawki (ML/data scientist): Big data and AI/ML analytics
Erica Jones (patient navigator): Recruitment, community deployment
Mehdi Khantan (electrical engineer): signal processing, firmware development
The Vision Forward
We see a continuum:
Today: NuroSleeve and similar devices reaching community users
Near-term: iBCI-ready platforms compatible with Precision and other implants
Mid-term: Living electrodes and biological interfaces (collaboration with Cullen Lab)
Long-term: Virtual white matter networks, peritoneal constructs, entirely biological restoration systems
From immediate assistive technology through rebuilding the injured brain with living neural tissue, we're committed to restoring independence and opening doors to entirely new human capabilities.




Comments